Pregnancy is a beautiful and transformative journey for women, but it can also bring about various health challenges. One such challenge is Gestational diabetes in pregnancy, a condition that affects pregnant women. In this article, we will explore what gestational diabetes is, its causes, risk factors, and most importantly, how to manage and maintain a healthy pregnancy while dealing with this condition.
What is Gestational Diabetes?
Gestational diabetes mellitus (GDM), also known as gestational diabetes in pregnancy, is a type of diabetes that develops during pregnancy. It typically occurs in the second or third trimester and can affect any pregnant woman, regardless of her pre-pregnancy health.
The condition is characterized by high blood sugar levels and is caused by the body’s inability to produce enough insulin to meet the increased demands during pregnancy.
Causes of Gestational Diabetes in Pregnancy
The exact cause of gestational diabetes isn’t fully understood, but several factors contribute to its development. Some of the key factors include:
- Changes in Hormones: During pregnancy, the placenta generates hormones that can interfere with the body’s capacity to utilize insulin properly. This hormonal shift can lead to elevated blood sugar levels, a key way in which gestational diabetes affect pregnancy.
- Insulin Resistance: Some women may have pre-existing insulin resistance, making them more susceptible to gestational diabetes. Insulin resistance occurs when the body’s cells don’t respond well to insulin, requiring the pancreas to produce more to maintain normal blood sugar levels.
- Genetic Predisposition: A family history of diabetes can increase the risk of gestational diabetes. If close family members have had diabetes, it’s essential to be more vigilant during pregnancy.
- Obesity: Being overweight or obese before pregnancy can increase the risk of developing gestational diabetes. Excess body fat can cause insulin resistance, making it harder for the body to manage blood sugar levels.
- Age: Women over the age of 25 are at a higher risk of developing gestational diabetes. The risk rises with age, particularly for women over 35.
- Previous Gestational Diabetes: Women who had gestational diabetes in pregnancy during a previous pregnancy are at a higher risk of developing it in subsequent pregnancies.
Risk Factors
While the causes of gestational diabetes in pregnancy are multifactorial, several risk factors increase a pregnant woman’s susceptibility to the condition. It’s important to be aware of these risk factors, which include:
- Obesity: A BMI above 30 significantly increases the risk of gestational diabetes.
- Age: Women aged 25 and older are more likely to develop gestational diabetes.
- Family History: A family history of diabetes, especially in close relatives, raises the risk.
- Ethnic Background: Some ethnicities, such as African American, Hispanic, Native American, and Asian American, have a higher prevalence of gestational diabetes.
- Previous Gestational Diabetes: A previous occurrence of gestational diabetes increases the risk for future pregnancies.
- Polycystic Ovary Syndrome (PCOS): Women with PCOS have a higher risk due to insulin resistance.
Managing Gestational Diabetes
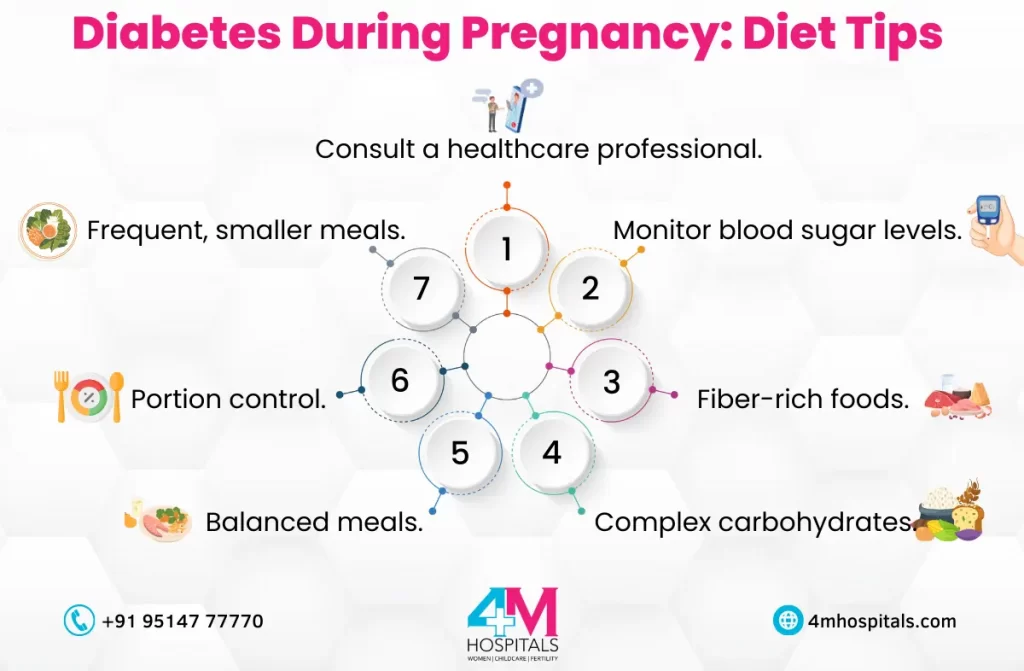
The good news is that with proper management, most women with gestational diabetes in pregnancy can have a healthy pregnancy and deliver a healthy baby. The key to managing gestational diabetes is maintaining stable blood sugar levels. Here are some strategies for doing so:
- Regular Monitoring: Monitoring your blood sugar levels regularly is crucial, especially since gestational diabetes affects pregnancy. Your healthcare provider will guide you on when and how to check your blood sugar levels. Keeping a record will help you and your healthcare team make necessary adjustments to your treatment plan.
- Healthy Eating: A balanced diet is essential for managing gestational diabetes in pregnancy. Consume a range of nutrient-dense foods, such as whole grains, lean proteins, fruits, and vegetables, and healthy fats. Avoid or limit high-sugar and high-carb foods.
- Portion Control: Watch your portion sizes to prevent blood sugar spikes. Smaller, more frequent meals can aid with blood sugar regulation. Regular physical activity can help reduce blood sugar levels. Consult your healthcare provider for a safe and suitable exercise routine during pregnancy.
- Medication if Necessary: In some cases, lifestyle changes may not be sufficient to control blood sugar levels. In these instances, medication, such as insulin, may be prescribed by your healthcare provider.
- Self-Care: Reducing stress and getting enough rest are vital components of managing gestational diabetes. Stress can impact blood sugar levels, so incorporating stress-reduction techniques like deep breathing or prenatal yoga can be helpful.
- Regular Prenatal Checkups: Attend all your prenatal checkups as scheduled during gestational diabetes in pregnancy. Your healthcare team will closely monitor your health and the baby’s development.
The Importance of a Healthy Pregnancy
Gestational diabetes in pregnancy can be challenging, but it’s important to remember that a healthy pregnancy is still very much attainable. Taking care of yourself and managing your blood sugar levels not only benefits you but also ensures the well-being of your developing baby. Uncontrolled gestational diabetes can result in a number of issues, such as:
- Large Birth Weight: High blood sugar levels can cause the baby to grow excessively, increasing the risk of birth injuries.
- Preterm Birth: Women with gestational diabetes are more likely to have preterm births.
- Low Blood Sugar in the Baby: After birth, the baby might experience low blood sugar levels, which can be dangerous if not managed promptly. Gestational diabetes in pregnancy poses risks to both mother and baby, emphasizing the vital need for vigilant monitoring and care during this critical period.
- Jaundice: Babies born to moms who have gestational diabetes are more likely to have jaundice.
- Preeclampsia: There is a higher risk of developing preeclampsia, a serious condition that can affect both mother and baby.
- Future Health Concerns: Women who’ve had gestational diabetes have a higher risk of developing type 2 diabetes later in life.
Conclusion
Gestational diabetes in pregnancy is a challenging condition, but it can be managed effectively with the right approach. By understanding the causes, risk factors, and effective management strategies, women can navigate pregnancy with gestational diabetes and still have a healthy, positive experience. Remember that working closely with your healthcare provider and adopting a healthy lifestyle can make all the difference in ensuring a safe and successful pregnancy.
Also Read Normal Delivery Hospital In Chennai.





